Autumn 2023
Supportive care for cancer patients requires a focus that assesses appropriateness, costs and the total impact on a patient’s care journey.
Supportive care for cancer patients addresses a number of issues such as ancillary conditions due to cancer treatments including neutropenia or bone metastases, side effects and symptoms like pain or nausea and emotional issues such as sadness or anxiety. Appropriate supportive care has numerous benefits including “decreased morbidity, improved quality of life and potentially decreased mortality.” In addition, there can also be decreased utilization of “healthcare resources and improved treatment outcomes.”1
Nevertheless, unmonitored supportive care can be problematic if a patient does not experience anticipated results from a particular course of care. As a result, supportive care drugs should be continually re-evaluated in light of the changes in courses of treatment. For example, once a patient starts treatment with colony stimulating factors (CSFs) for prophylaxis of neutropenia, it is often continued for the entirety of their treatment course. However, the use of CSFs needs to be re-evaluated once the patient discontinues the treatment that required empiric CSFs therapy.
Even more concerning is the inappropriate use of supportive care drugs that are not guideline compliant or evidence based. When supportive therapies are improperly used there are a number of negative effects that should be considered (see Sidebar). In addition, not only are supportive care medications that are improperly prescribed wasteful, but these medications may also adversely impact the patient’s well-being (see Sidebar).
Sidebar: Appropriateness and Usage
One issue that clinicians have noted is the side effects attached to the use of some supportive care drugs. In some patient cases, CSFs have been known to contribute to cancer growth.2 Moreover, CSFs can cause additional side effects such as bone or muscle pain, fatigue, nausea and diarrhea.3 Patients with castrate-sensitive prostate cancer who have bone metastasis can be improperly prescribed bone agents such as Denosumab which has been shown to only be effective in castrate-resistant prostate cancer patients with bone metastasis.4 Not only is that drug not NCCN compliant for castrate sensitive prostate cancer, it is significantly more expensive than other bone agents (see Spotlight). Finally, the optimal duration of therapy for either Denosumab or Zoledronic acid remains uncertain, so patients should be monitored for the effectiveness of this treatment.
Spotlight: Cost Considerations
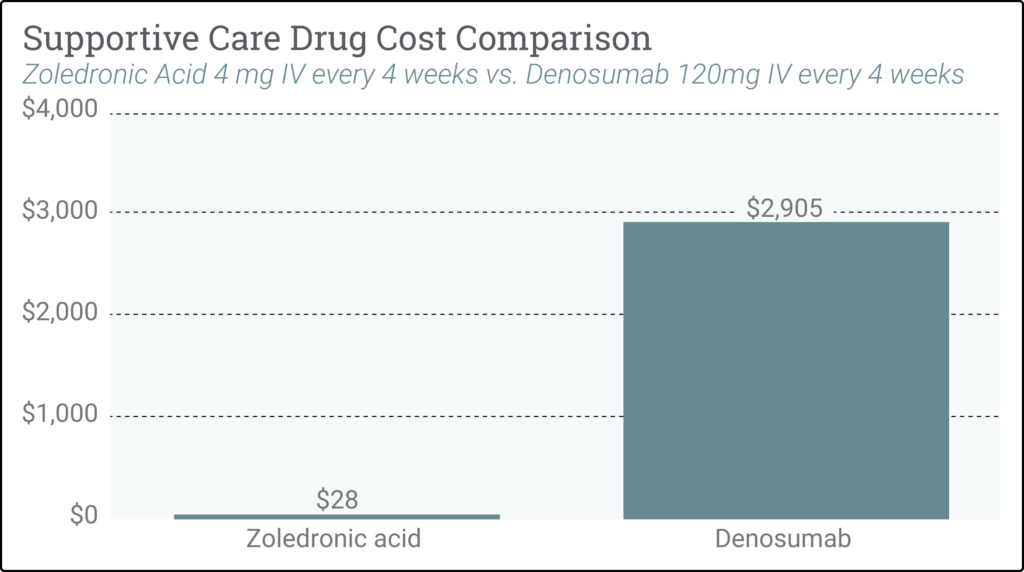
The accompanying graph illustrates the significant cost differential between Denosumab vs. Zoledronic Acid used for patients with solid tumor cancers who have bone metastasis. Both can be used for bone metastasis; however, if the patient does not have a renal contraindication, zoledronic acid is as clinically effective and more cost efficient than Denosumab.*
* Pricing is from the October 2023 CMS ASP pricing schedule
For further information, please contact:
Adam Goldston (email)
Chief Growth Officer
OPN Healthcare